How to Manage PGAD/GPD with Expert Guidelines
Feb 06, 2026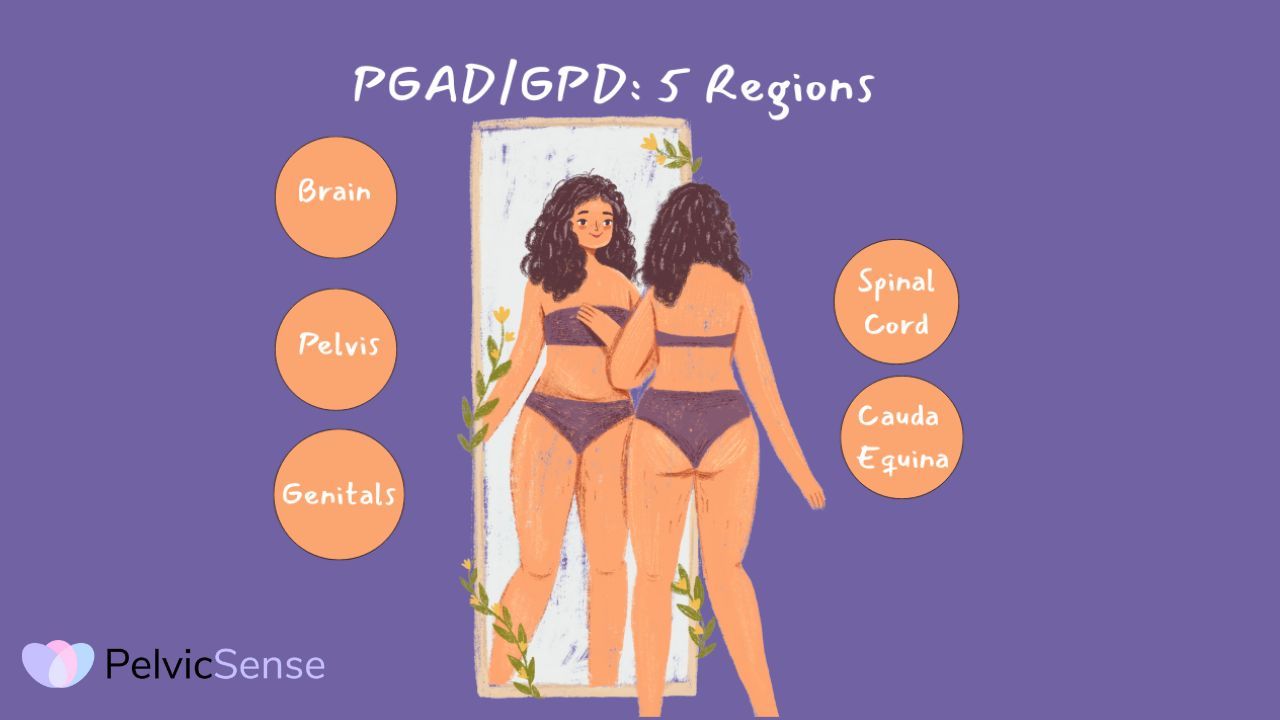
Key Takeaway:
PGAD/GPD is a real medical condition affecting all genders, characterized by persistent, unwanted genital sensations that occur without sexual desire. It's not hypersexuality or a psychological problem. The core mechanism is central sensitization, where the nervous system becomes hypersensitive and amplifies signals, like chronic pain conditions.
Triggers can originate from multiple body regions including the genitals, pelvis, spine, and brain (including medications like SSRIs/SNRIs). Evidence-based treatment emphasizes psychological intervention as first-line care combined with pelvic floor therapy, addressing nervous system dysregulation, fear, and hypervigilance. Finding an informed healthcare provider is critical studies show that provider helpfulness directly reduces symptom severity and improves outcomes.
What is PGAD (Persistent Genital Arousal Disorder)?
PGAD is a distressing medical condition characterized by persistent, unwanted genital sensations that occur without sexual desire, interest, or fantasies.
What is GPD (Genito-Pelvic Dysesthesia)?
GPD stands for Genito-Pelvic Dysesthesia, an alternative term for the same condition as PGAD
PGAD Symptoms and Sensations
PGAD/GPD involves ongoing or recurring, unwanted and distressing sensations of genital arousal that last for at least three months. These sensations can include:
- Feelings of being on the verge of orgasm
- Tingling, throbbing, buzzing, or pulsating
- Swelling or contractions
- Other uncomfortable sensations like burning, twitching, itching, or pain
It’s important to understand that these sensations occur without any sexual desire, thoughts, or fantasies. This is not hypersexuality or sex addiction. You are not experiencing sexual desire; instead, you are having unwanted and distressing physical sensations.
PGAD in males and in females
While most research on PGAD/GPD has focused on women, recent studies show that it affects people of all genders:
- Women: 0.6% to 3.0% may experience PGAD Symptoms
- Men: 1.1% to 4.3% may experience these symptoms
- Gender-minoritized individuals: Also affected, though less research is available
How the Brain and Nervous System Cause PGAD Symptoms
Researchers have found a key factor called central sensitization. Think of it as an alarm system stuck in the “on” position.
Here's what happens:
Over time, the nervous system and immune system can become overly sensitive to threats, whether they are emotional, psychological, social, or physical. When this happens, your brain believes you are in danger and sends distressing sensations as a way to protect you.
This process is known as central sensitization. It means that neural signals in the central nervous system (the spinal cord and brain) become amplified, leading to increased sensitivity to pain. In this context, “pain” refers to any ongoing, distressing sensation.
Even when nothing is touching or stimulating your genitals, your brain can send alarm signals that cause sensations like unwanted arousal, pain, urgency, burning, and more.
This helps explain why mind-body treatments may be effective. They help calm the overactive nervous and immune systems, making it easier for the brain to receive signals of safety.
Cross-Sensitization: Why Symptoms Spread
You might notice that these sensations do not stay in one place. They can occur in your genitals, but also in your bladder, lower back, legs, or other areas. This is called cross-sensitization.This happens because nerves from different parts of the body meet in the spinal cord.
If one area, such as the genital region, becomes sensitized, it can change how you feel sensations in other areas. That’s why PGAD/GPD symptoms can affect several, seemingly unrelated, parts of the body.
The Healthcare Challenge You're Facing
It can be difficult to find healthcare providers who understand this condition. Recent research found:
- 40% of people waited 6 months or more before approaching a healthcare provider
- About 50% consulted with at least 6 different providers before finding help
- 17% still haven't approached a provider due to shame and embarrassment
The most common barriers? Healthcare providers' lack of knowledge about PGAD/GPD, providers not acknowledging the distress it causes, and patients' own discomfort discussing symptoms.
One important finding is that patients who felt their provider was helpful reported less severe symptoms. This shows how important it is to find the right support.
New Guidelines: The 5-Region Diagnostic Approach
The 2026 expert consensus introduces a new way to diagnose PGAD/GPD by finding out where in the body the trigger starts. Knowing this can help guide the best treatment.
The 5 Regions:
Region 1: End Organ (Genitals Themselves)
Triggers may include inflammation, nerve problems, skin conditions, or hormonal issues affecting the clitoris, penis, vulva, scrotum, vestibule, urethra, bladder, vagina, or prostate.
Region 2: Pelvis/Perineum Triggers may include:
- High-tone pelvic floor dysfunction (tight pelvic floor muscles)
- Pudendal nerve problems
- Pelvic vein disorders (varicose veins in the pelvis
Region 3: Cauda Equina (Lower Spine Nerve Roots) Triggers may include:
- Tarlov cysts (fluid-filled sacs on spinal nerve roots)
- Herniated discs in the lower back
- Annular tears (tears in spinal discs)
Region 4: Spinal Cord
Triggers may involve inflammation or problems in the spinal cord pathways above the lower spine.
Region 5: Brain Triggers may include:
- Medications (especially starting or stopping SSRIs/SNRIs, or using trazodone)
- Brain injuries or conditions
- Psychological factors (stress, anxiety, history of trauma)
It’s important to know that you may have triggers in more than one region. That’s why a thorough evaluation is needed.
Treatment Recommendations: What Actually Helps
Psychological Approaches (Strongly Recommended Throughout Treatment)
The expert panel strongly recommends using psychological support alongside other treatments throughout the whole process.
Why psychology first?
- It’s safe and does not carry the risk of making symptoms worse, unlike some medications.
- It addresses the root problem by targeting the overactive nervous system and central sensitization.
- It helps reduce distress. Many people with PGAD/GPD experience high levels of anxiety, depression, and sometimes even suicidal thoughts.
- It is effective. Research shows that reducing worst-case thinking, fear, and constant monitoring of symptoms leads to better outcomes.
What psychological treatment includes:
- Cognitive Behavioral Therapy (CBT): Helps you identify triggers, challenge catastrophic thoughts, and develop coping strategies
- Mindfulness practices: Helps you relate differently to sensations without judgment or fear
- Stress management: Reduces nervous system activation that can fuel symptoms
- Trauma-informed care: If you have a history of sexual abuse (reported in about 50% of cases), addressing this is important
Research shows that: people who learned to worry less, stop constantly checking their symptoms, manage stress, and stay involved in daily activities had fewer symptoms and a better quality of life.
Pelvic Floor Physical Therapy (Recommended Concurrently)

Pelvic floor physical therapy is recommended as a first step alongside psychological care, especially if you have tight pelvic muscles.
Treatment may include:
- Manual therapy to release tight muscles
- Biofeedback
- Therapeutic exercises to promote relaxation
- Treatment of related areas (hips, spine, breathing)
For some people, specialized treatments like TENS (transcutaneous electrical nerve stimulation) or Botox injections into the pelvic floor muscles may be helpful.
Medical Treatments and Specialized Procedures for PGAD/GPD
Depending on the specific triggers identified through comprehensive evaluation, medical treatments may include:
- Medications: While there are no medications specifically approved for PGAD/GPD, some may help manage symptoms when prescribed by experienced healthcare providers. It’s important to note that certain medications, especially some antidepressants, can sometimes trigger or worsen PGAD/GPD symptoms. Any medication decisions should be made carefully with a provider who understands this condition.
- Specialized Procedures: For people with specific identified causes (such as nerve compression, spinal issues, or vascular problems), targeted procedures may provide relief. These are typically considered after psychological and physical therapy approaches have been tried.
The expert panel highlights that more than one region or trigger may be involved, and most people benefit from a combination of different therapies.
Why Self-Care Programs Are So Important
This is where structured self-care programs become essential.
What Self-Care Can Do for You
A good home program teaches you to:
- Track what makes symptoms better or worse
- Practice pelvic floor exercises that may help reduce tension
- Learn calming techniques (breathing, relaxation, mindfulness)
- Challenge worried thoughts that increase nervous system activation
- Shift your attention away from symptoms
- Build your own toolkit of strategies that work for you
Research shows that people who use these programs often feel less distress, worry less about their symptoms, and see improvements in anxiety and depression. The key is to practice regularly. People who did the exercises consistently reported feeling better
The PelvicSense Approach
At PelvicSense, our comprehensive self-care programs are specifically designed to address PGAD/GPD using evidence-based approaches that include:
- Pelvic floor education and down-training exercises
- Stress management and nervous system regulation techniques
- Cognitive strategies to reduce catastrophizing and hypervigilance
- Practical tools for managing symptom flare-ups
- Guidance on when and how to seek additional professional support
Self-care programs may not replace professional therapy for everyone, but they can be a helpful first step, a complement to other treatments, or an accessible option when specialized care is not available right away.
A self-care home program can be particularly beneficial as:
- A starting point while you search for a knowledgeable provider
- An ongoing complement to medical treatments
- A maintenance strategy between therapy sessions
- An accessible option when financial or geographic barriers exist
When to Seek Additional Support
However, if you are experiencing severe depression, suicidal thoughts (which can affect up to 54% of people with PGAD/GPD), or symptoms that make daily life very difficult, it is important to seek professional mental health support as soon as possible.
How New Guidelines Help You Manage and Treat PGAD/GPD
The ICSM 2024 recommendations stress that treatment should use a comprehensive biopsychosocial model. This means:
- Start psychological interventions right away. They are safe, effective, and help address the nervous system’s role.
- Identify and treat specific triggers by using the 5-region diagnostic approach.
- Use multiple approaches simultaneously. Psychological support, physical therapy, and medical treatments can all work together, not doing one to see if it’s effective
- Make sure the treatment plan is tailored to you, since what works can vary from person to person.t These New Guidelines Mean for You
The ICSM 2024 recommendations represent a major step forward in:
- Recognizing PGAD/GPD as a legitimate medical condition affecting all genders
- Providing clear diagnostic guidelines for healthcare providers
- Establishing evidence-based treatment recommendations
- Reducing the stigma and isolation that people with PGAD/GPD often feel
If you are living with PGAD/GPD, remember: symptoms are real and recognized by medical experts
- Effective treatments exist, particularly psychological and mind-body approaches
- Support and resources are available
- Self-care programs like those offered by PelvicSense can provide accessible, evidence-based support
Wrap Up
Managing PGAD/GPD can take time and may involve trying different approaches. With the right support and tools, improvement is possible.
This blog is based on "Persistent genital arousal PGAD disorder/Genito-pelvic dysesthesia in all genders: recommendations from the Fifth International Consultation on Sexual Medicine (ICSM 2024)," published in Sexual Medicine Reviews, January 2026.
References
The recommendations in this article are based on the consensus of international experts from multiple disciplines, including gynecology, neurophysiology, pelvic floor physical therapy, psychology, sexual medicine, and urology, who reviewed the literature and developed evidence-based guidelines at the International Consultation on Sexual Medicine in Madrid, June 2024.
DOI: 10.1093/sxmrev/qeaf082
Direct link: https://academic.oup.com/smr/article/14/1/qeaf082/8436914

