Hypertonic Pelvic Floor Relief: How to Calm Your Nervous System and Reclaim Your Life
Jan 26, 2026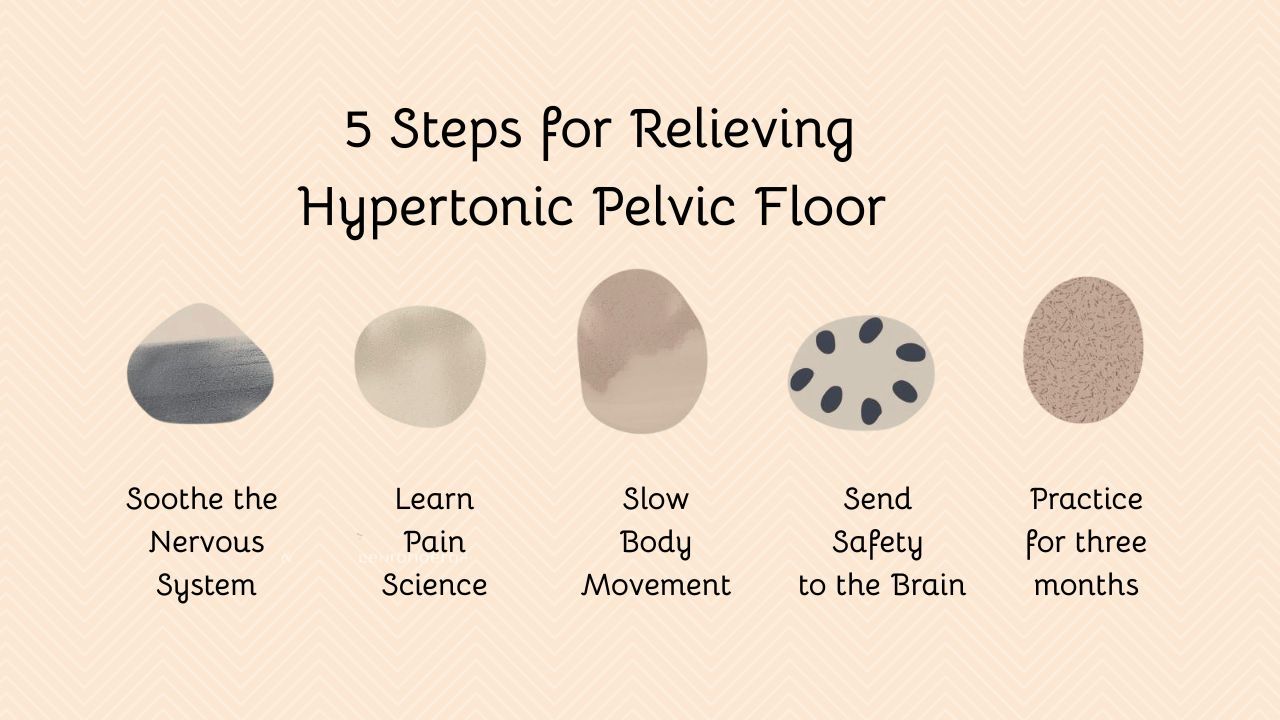
Key Takeaway:
Ongoing pelvic tension and pain can feel isolating and confusing, especially when treatments haven’t worked. A hypertonic pelvic floor means your nervous system has learned to stay on guard, often because of stress or past pain. The good news: this protective pattern can be unlearned. Real relief comes from teaching your brain that your pelvis is safe again, through gentle, science-based self-care that calms both body and mind.
Understanding the Hypertonic Pelvic Floor
A hypertonic pelvic floor means the pelvic muscles remain tense and do not relax easily. This tension often leads to hypertonic pelvic floor symptoms such as pelvic pain, pain during sex, frequent urination, constipation, or tailbone pain.
Many people think that tight muscles just need to be stretched or released. While hands-on therapy and movement can help, this is often not enough, especially if symptoms have lasted for months or years.
If you have already tried treatments and tests, it helps to know this: your pain does not mean your body (muscles, organs, nerves) is damaged. It means your system is trying to protect you.
When the body is healthy, the nervous system, immune system, and brain work together like a security system. When an injury occurs, the alarm activates to protect and support healing. In chronic pelvic pain, this system can become overly sensitive and react even without real danger. This is known as central sensitization (Woolf, 2011).
Stress-related pelvic pain does not mean something new is wrong. It means your nervous system is reacting to perceived danger. This reaction can be changed.
This is why some people still have symptoms after surgery or medication. Their nervous system hasn't learned that the pelvis is safe. An effective hypertonic pelvic floor treatment must focus on the brain and spinal cord, which amplify threat signals.
The Role of Central Sensitization in Pelvic Pain
Central sensitization occurs when the brain and spinal cord amplify the perception of threat signals, whether the threat is real or merely expected (Woolf, 2011). Over time, the pain you feel and the muscle tension you experience may no longer match what is happening in your tissues. Instead, your nervous system is picking up too many threats, sending them to the brain.
The brain has learned to create these symptoms by sending pain chemicals to areas where you have had prior issues, as a way to guard you from perceived danger.
In people with chronic pelvic pain, this may show up as:
- Pain that seems disproportionate to exam findings
- Multiple pelvic diagnoses over time
- Sensitivity to touch, pressure, or internal exams
- Worry about movement, intimacy, or bodily sensations
- Sleep disruption and fatigue
- Concern about pain worsening or moving to different areas
Here is how the cycle often works:
- Stress signals danger
- The brain tightens the pelvic muscles
- Tension reduces oxygen and creates discomfort
- The brain notices the discomfort and increases protection
- Pain increases even without injury
Many people experience this exact cycle
Understanding this process can help you feel more in control. It shows that your symptoms are real, not imagined, and that you can work toward pelvic wellness.
5 Proven Steps to Finding Relief
Step 1: Shift the Goal From Relaxing the Muscles to Calming the Nervous System
If you try to force your pelvic muscles to relax, they can actually get tighter. Your nervous system needs to feel safe before your muscles can let go.
If you are unsure where to begin, start with breathing. It is the fastest way to calm the nervous system. Once breathing feels familiar, add mindfulness and body awareness. Movement comes later, not first.
Practices that support parasympathetic (rest-and-digest) activation include:
- Slow diaphragmatic breathing
- Extended exhalation breathing
- Gentle body scanning
- Mindfulness-based awareness
Practicing these techniques for a few minutes each day over several months can help reduce threat signals to the brain. Over time, your pelvic floor muscles will start to relax as your brain senses you are safer, like a well-practiced response that creates calm under stress.
Studies show that breathing and mindfulness can lower pain and improve quality of life for people with chronic pelvic pain by calming both the nervous and immune systems (Fitzgerald et al., 2013).
Step 2: Reframe Pain Through Pain Science Education
Learning about pain and ongoing pelvic symptoms, such as urgency, burning, and abdominal discomfort, helps people understand that these symptoms do not always mean there is tissue damage. When pain or discomfort lasts a long time, it is often because the brain perceives too many threat signals and responds with protective symptoms.
Learning how pain works can:
- Reduce fear and catastrophizing
- Improve confidence in movement
- Decrease avoidance behaviors
- Enhance engagement in recovery
Research shows that learning about pain, along with doing mind/body self-care, can lower pain and disability (Louw et al., 2011). A study of the PelvicSense digital home program showed a significant reduction in pain intensity and catastrophization by women with different chronic pelvic pain diagnoses after 3 months of use.
Learning how the brain and pelvis are connected can help you feel more hopeful and take an active role in your recovery.
Step 3: Introduce Gentle, Non-Threatening Movement
Movement is vital, but the pace matters. When selecting exercises for hypertonic pelvic floor muscles, the focus should be on:
- Slow and mindfulness
- Coordinated with breathing
- Free of performance pressure
- Focused on feeling safe rather than on intense stretching sensations
Methods like graded motor imagery and slow, steady exposure help the brain get used to pelvic movement without causing the muscles to tense up.
This process is not just about making your muscles stronger. It is about retraining how your brain and pelvic floor communicate with each other.
Step 4: Address Fear, Intimacy, and Pelvic Function Without Pressure
Fear and worry about activities like sex, medical exams, using the bathroom, or feeling the frequent urge to urinate can keep the nervous system in a protective state. When your brain perceives these activities as threats, it keeps the pelvic floor tense as a protective response.
Reducing this fear is essential for recovery. This is where the self-soothing practices from Step 1 become your most powerful tool. When you weave breathing, body scanning, and mindfulness lightly throughout your day, you are consistently sending safety signals to your nervous system. Over time, this steady practice helps reduce the fear response.
This process involves:
- Approaching feared activities gradually, without forcing yourself
- Removing pressure and expectations from yourself
- Using your calming practices before, during, or after challenging activities
- The goal is not to rush your recovery or force yourself into uncomfortable situations.
Instead, you are gradually teaching your brain that these activities are safe. As your sense of threat decreases, your pelvic floor will naturally begin to relax.
This is your nervous system relearning what safety feels like.
Step 5: Commit to Consistent Practice Over Time
If this feels overwhelming, remember: it takes time to change how your nervous system responds.
Research on neuroplasticity shows that steady, repeated practice for about three months is often needed before you notice real changes (Moseley & Butler, 2017). This is why performing your hypertonic pelvic floor exercises daily is so important. At this stage, the goal of movement is not physical fitness. It is about building new neuronal connections and safer habits.
Patients benefit when clinicians:
- Normalize the time course
- Emphasize patience and consistency
- Reinforce small wins
- Encourage ongoing self-management
Sticking with your practice is more important than doing it perfectly.
Why a Mind-Body Approach Works
A medical approach alone often misses how the nervous, immune, and brain systems can keep the pelvic floor tense. Mind-body strategies help because they address:
- Neural threat detection
- Autonomic regulation
- Emotional processing
- Learned pain patterns
These methods are not meant to replace medical care or pelvic physical therapy. Instead, they add to your care by addressing the main causes of ongoing pain or distressing symptoms (Moseley & Butler, 2017).
Digital home programs, with clinician support, can help you stick with self-management and keep making progress when in-person visits are not possible.
FAQs
What is hypertonic pelvic floor?
A hypertonic pelvic floor occurs when the muscles in the pelvic base stay contracted and cannot relax. While many people focus on strengthening these muscles, a hypertonic state means they are already overactive or too tight.
When these muscles are constantly tense, they lose their ability to function correctly, which often leads to pain or discomfort in the pelvic region.
What are the causes of hypertonic pelvic floor?
Chronic stress and anxiety are common causes because the body holds tension in the pelvic muscles. Intense exercise or constant core gripping also leads to tightness. Some people develop it as a protective response to pain or surgery. Poor posture and shallow breathing habits are other common factors.
How to relax your hypertonic pelvic floor?
To relax these muscles, practice deep diaphragmatic breathing to help the pelvic floor drop and soften naturally. You can also incorporate gentle stretches like child's pose and happy baby to release tension. Avoid habits like sucking in your stomach or gripping your glutes throughout the day. For the best results, consult a pelvic floor physical therapist for personalized manual release techniques.
How to fix hypertonic pelvic floor?
Fixing a hypertonic pelvic floor requires a whole‑person approach rather than a quick fix. Effective recovery includes pain science education, nervous system regulation, gentle movement, and addressing fear related to pelvic sensations.
Working with a pelvic health professional and following a structured, mind‑body‑based program can help retrain the brain and muscles to return to a normal resting state. With steady practice over time, the pelvic floor can relearn how to relax and function comfortably again.
Final Thoughts
A hypertonic pelvic floor is not a personal failure, a weakness, or proof that you cannot heal. It simply means your nervous system, immune system, and brain have learned a pattern to protect you, and this pattern can be unlearned.
Real recovery happens when you stop focusing only on fixing the pelvis and start helping your brain learn that the pelvis is safe. PelvicSense is an easy-to-follow guide to achieve this goal.
With learning gentle movement calming your nervous system, and steady practice your body can learn to relax again. Relief may take time, but it is possible.
Pelvic wellness starts by creating conditions that support safety, comfort, and lasting healing.
Scientific References
- Woolf, C. J. (2011). Central sensitization: implications for the diagnosis and treatment of pain. Pain, 152(3), S2-S15.
- Moseley GL, Butler DS. Explain Pain. Noigroup Publications.
- Louw, A., Diener, I., Butler, D. S., & Puentedura, E. J. (2011). The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiotherapy Theory and Practice, 27(5), 363-384.
- Fitzgerald, M. P., Anderson, R. U., Potts, J., Payne, C. K., Peters, K. M., Clemens, J. Q., ... &
- Nyberg, L. M. (2013). Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. The Journal of Urology, 189(1), S75-S85.

