Your Pelvis Could Hold the Key to Healing Chronic Lower Back, Hip and Foot Pain
Jul 05, 2022
The Cause of Pelvic Floor Dysfunction in Back, Hip, and Foot Pain
If chronic back pain, hip pain, or foot pain hasn’t improved with standard orthopedic care, your pelvic floor may be the missing piece. Watch for signs like pain that worsens during the day, pelvic heaviness, pain with sex, or unexplained foot pain, and consider pelvic focused rehab that includes breathing, nervous system retraining, and gradual movement to address the root cause, not just the symptoms.
Introduction:
Chronic back, hip, and foot pain are often treated as isolated orthopedic problems, yet many people continue to struggle despite medications, physical therapy, and specialist care. What’s rarely discussed is that these pain patterns can be closely connected to the pelvic floor, especially when symptoms are persistent, vague, or difficult to pinpoint. Because pelvic and genitourinary symptoms are uncomfortable to talk about, they’re frequently overlooked, even though they can provide important clues.
Understanding the role of pelvic floor dysfunction can help explain why pain may travel between the lower back, hips, and feet, and why healing sometimes requires looking beyond the site of pain itself. This article explores how the pelvic floor influences core stability, hip mechanics, and even foot pain, and what you can do when traditional treatments haven’t brought lasting relief.
Lower Back Pain
Based on the type of discomfort you’re experiencing, the cause may be the pelvic floor. In his article: ‘Musculoskeletal Causes of Chronic Pelvic Pain’, Dr. Anthony Gyang reports when lower back pain feels vague and poorly localized, one-sided, aching, throbbing, and/or heavy, this might indicate that pelvic dysfunction is the cause. In addition, you may experience a sensation of pelvic floor heaviness or pressure.
Signs that your pain may be connected to a ‘hypertonic’ or ‘tight’ pelvic floor include acute attacks of pain that awaken you at night, radiation of the pain to your sacrum, and pain with sex. In women, this is often referred to as dyspareunia. For men, it may manifest as erectile dysfunction.
Low back pain that starts in the afternoon and gets progressively worse as the day goes on may indicate the presence of ‘Levator Ani Syndrome’, and overly tight pelvic floor muscles. These flares may be constant for days at a time or occur suddenly with a short duration.
The reason for this relationship has to do with the role the pelvic floor plays in stabilizing your core. During many activities, your deep fibers of the lower back muscles, abdominal muscles, and pelvic floor work together as a 3-point brace to keep your spine stable. When one of these muscles malfunctions, it can put stress on the other two, resulting in pain.
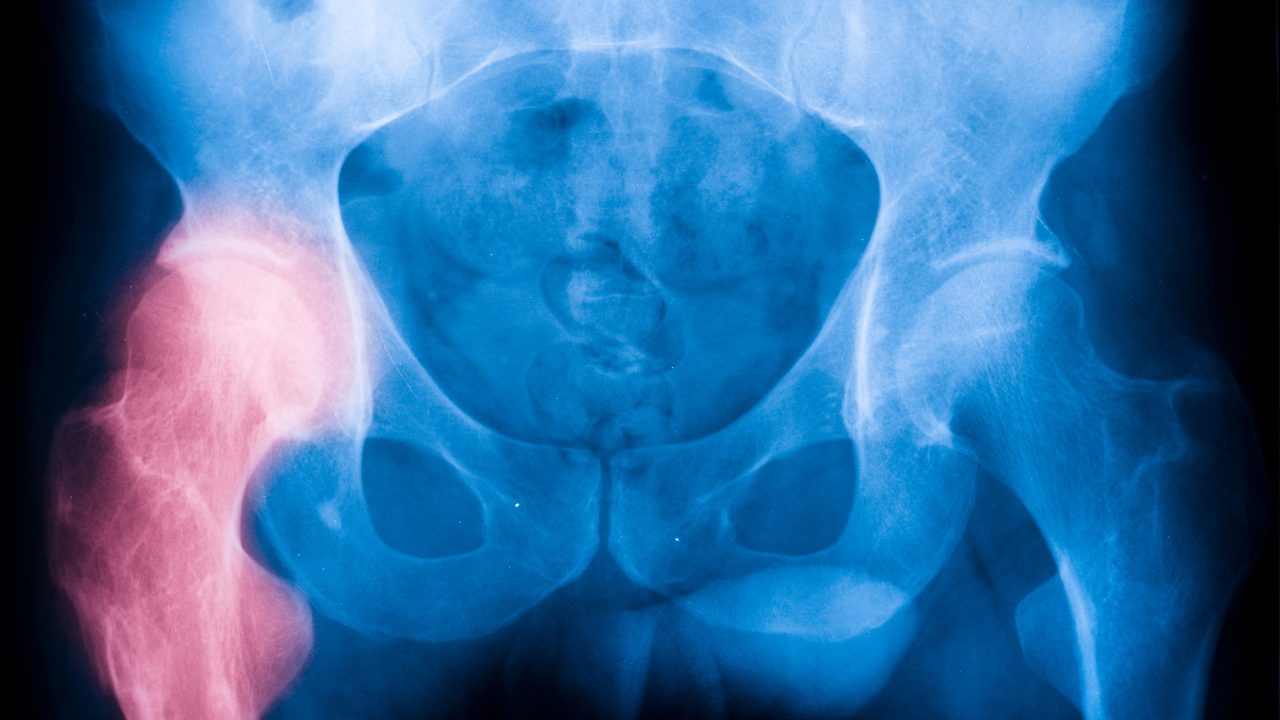
Hip Pain
The deep hip muscles that provide hip stability and rotation motion have attachments onto the pelvic floor muscles! So if you're experiencing chronic hip pain, there may be an underlying pelvic floor component.
Three common causes of hip pain include hip osteoarthritis, labral tears and femoroacetabular impingement (hip impingement). Each condition reflects a deviation from proper hip biomechanics and may be influenced by dyssynergic (improperly functioning) musculature. Two of the muscles that are both part of the pelvic floor and help control our hips are the Piriformis and the Obturator Internus. Both of these muscles assist in rotating the leg out and in stabilizing the head of the femur into the hip socket. If the hip socket is unstable, it can cause stress to these muscles, thereby causing stress to the pelvic floor as a whole, and vice versa.

Foot and ankle pain
The connection between the ankle/foot and the pelvic floor is offering more insights into healing chronic foot and pelvic pain.
Several studies now link increased activity of the ankles to increased activity of your pelvic floor muscles. When the mechanics of your lower legs are changed due to an ankle sprain, flat feet, fractures, or other foot and ankle conditions, it’s likely that the activity of your pelvic floor musculature may be affected as well.
In addition, if you’re experiencing foot pain and having difficulty identifying the cause, there may be a phenomenon known as “smudging” happening in the brain.
Your brain has a virtual map of your body so the brain knows what’s happening to each part of your body. This area is called the Sensorimotor Cortex. Hundreds of thousands of brain cells or neurons represent each of our body parts.
So where is the foot/ankle on our brain’s virtual map? Right next to the genital/pelvic region!
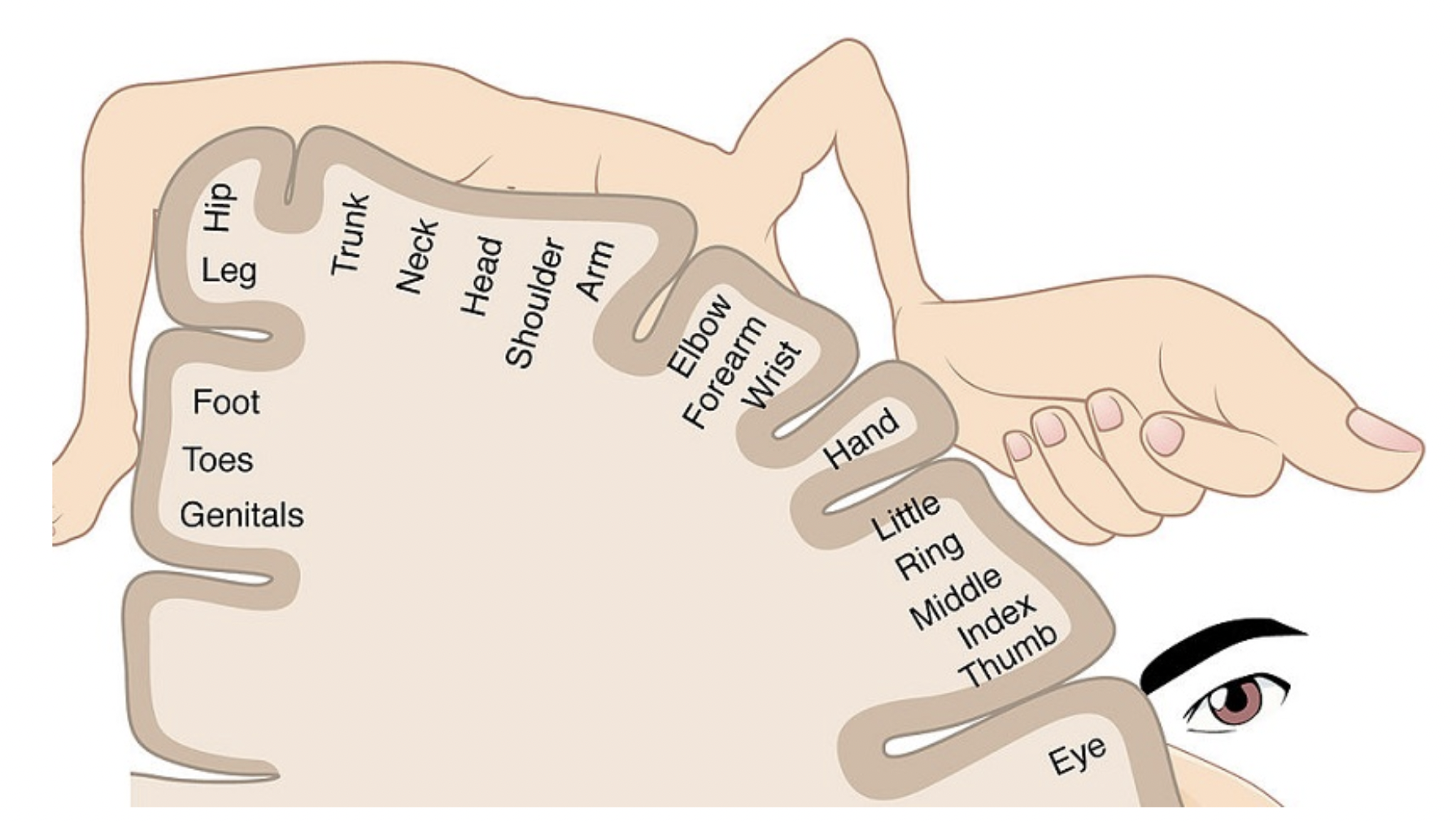
When you’ve experienced foot pain for long periods of time, your brain may begin to “smudge” the neurons that represent the pelvic area or vice versa.
The good news is that the brain and nervous system can be retrained (due to its neuroplasticity) and healing can be achieved no matter how long you’ve suffered from persistent pain.

Conclusion
When chronic back, hip, or foot pain refuses to improve, it’s often a sign that the real issue hasn’t been addressed yet. The pelvic floor sits at the center of core stability, hip control, and pain signaling, which means dysfunction here can quietly drive symptoms far beyond the pelvis. What feels like a stubborn orthopedic problem may actually be a coordination issue involving muscles, nerves, and the brain.
Lasting relief comes from treating the body as an integrated system, not a collection of disconnected parts. By addressing pelvic floor dysfunction, retraining the nervous system, and restoring healthy movement and breathing patterns, it’s possible to reduce persistent pain and regain confidence in your body again. For many people, this shift in focus is the turning point that finally moves them out of the chronic pain cycle.
References:
- Chen, H., Lin, Y., Chien, W., Huang, W., Lin, H., & Chen, P. (2009). The Effect of Ankle Position on Pelvic Floor Muscle Contraction Activity in Women. Journal of Urology, 181(3), 1217-1223. doi:10.1016/j.juro.2008.10.151
- Prather, H. (2002). Musculoskeletal Evaluation for Pelvic Pain. Female Pelvic Health and Reconstructive Surgery, 241-261. doi:10.3109/9780203908938-16
- Pelvic, Sexual Intercourse, and Abdominal Pain can be Simple or Complex. (n.d.). Retrieved February 22, 2019, from http://pelvicexpert.com/readmore_pain.php
- Muscolino, J. (n.d.). Muscles of the Pelvis. Retrieved February 22, 2019, fromhttps://learnmuscles.com/blog/tag/obturator-internus/
- Vandyken, C., & Hilton, S. (2019). The Puzzle of Pelvic Pain: A Rehabilitation Framework for Balancing Tissue Dysfunction and Central Sensitization II: A Review of
- Gyang, A., Hartman, M., & Lamvu, G. (2013). Musculoskeletal Causes of Chronic Pelvic Pain. Obstetrics & Gynecology, 121(3), 645-650. doi:10.1097/aog.0b013e318283ffea Treatment Considerations. Journal of Womenʼs Health Physical Therapy, 36(1), 44-54. doi:10.1097/jwh.0b013e31824e0ab4
IMAGE CREDIT: ANATOMY & PHYSIOLOGY, CONNEXIONS WEBSITE. HTTP://CNX.ORG/CONTENT/COL11496/1.6/

